So, how did your insurance renewal season go? You likely spent a considerable amount of time collecting revenue and payroll forecasts, as well as details about your operations and assets. Time spent reviewing and completing those applications includes asking your operations team if anything plans to change during the next policy period. Like a long winter season, you are glad to see the insurance renewal season come and go.
During the renewal process, your broker may have presented part of your risk management strategy to new insurance carriers and their underwriters. They probably wanted to hear about some of your losses and how future losses will be mitigated. As a risk manager, you were able to articulate some new strategies for reducing general liability and property claims. Perhaps you presented your plan for reducing auto losses by showcasing your new fleet management program with lots of new training, accountability, and telematics.
Reflecting on the costs, data from the National Council on Compensation Insurance reveals that the average workers’ compensation claim cost was $41,757 in 2020-21. More severe injuries, such as fractures or burns, lead to even higher costs—up to $126.033 on average for the most severe cases. From this, it’s clear to see just how important diligent risk management and proactive safety measures are to mitigate such costs.
But could there be untapped potential to further enhance these outcomes? Are there overlooked strategies that could streamline your operations and improve your company’s risk profile? We’ll address these questions and more, offering insights and strategies to enhance your risk management efforts effectively.
The Role of Modern Risk Management in Better Workers’ Comp Outcomes
When it came to workers’ compensation, you touted your new initiatives for preventing workplace injuries, using a Safety Management System, and innovative products such as AI-enabled video monitoring and wearables. You may have even talked about your new internal claims manager or human resources professional who developed a great Return-to-Work program.
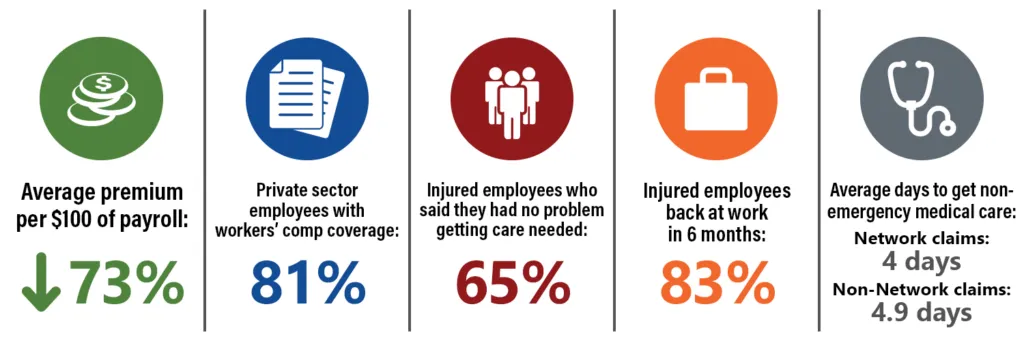
A missed opportunity for you and your company may be the ability to reduce workers’ compensation claim costs using modern technology. By leveraging telemedicine and near-instant access to a doctor, an injured worker can receive an assessment and treatment plan using their phone. This is a game-changer for the traditional response to workplace injuries, which often includes only basic on-site first aid. Oftentimes, workers are unnecessarily sent to urgent care centers and emergency rooms for minor injuries that could have been treated through telemedicine. By visiting an urgent care center or an emergency room, OSHA-recordable incident will likely be created, when in fact it likely could have been avoided. Typically, an injured worker will be accompanied by a supervisor, so you now have two workers off the job site for an extended period.
The Challenges from Injury to Recovery
The journey from the moment of injury to a return to work can often be a long one for both the injured worker and their employer. There can be delays on several fronts as each stakeholder works through the process of filing a claim, making referral and therapy appointments, seeking approvals, completing forms, etc. If the injured worker or their employer lose trust in one another, a claim can often drag on longer than it needs to. When that occurs, all stakeholders are at risk. Full recovery for the worker can take longer than it should, while the employer and insurance carrier will see the claim costs escalate unnecessarily.
Injury Investigation and Risk Analysis
Risk managers are excellent at performing a root-cause analysis of why a loss has occurred. They spend hours discussing losses with department managers, trying to get to the real root cause of why something negative has occurred within the organization. A good organization will have a focus on safety as part of their overall company culture. When an injury occurs, safety professionals, department managers, and risk managers work to find the root cause to prevent a similar occurrence in the future. These post-incident investigations and root-cause analysis exercises are important and necessary.
Workers’ Compensation Claim Costs
When it comes to workers’ compensation claims, have you ever found yourself in a claim review with your insurance carrier or third-party administrator (“TPA”) and wondered, “How did we get here? Why has this claim dragged on? Why is the injured worker so angry with everyone? Why are the medical and indemnity costs so high? Why did the worker feel like they needed legal representation?”
If you have ever found yourself asking these questions, did you attempt to do a root-cause analysis? If you did, were you able to acquire the necessary answers to the typical root-cause analysis question of “Why?” Typically, asking “Why” reveals the true answer after asking the question 4-5 times. With Workers’ Compensation claims, it can be difficult to ask questions of the representative stakeholders. Certainly, you can ask your internal claims manager or HR department, and perhaps the injured worker. However, it can be difficult or impossible to ask medical providers and insurance adjusters.
Workplace Injury Management Complexities
The issue with many workers’ compensation cases ties back to the first week after the injury occurred. Did the worker receive immediate care and treatment? Were referral and follow-up appointments easy to schedule and attend? Was there clear communication amongst all stakeholders? Excessive delays and a lack of communication can lead to the worker feeling lost in the process and will ultimately become disengaged and non-compliant with the recovery plan. Have you performed a root-cause analysis of claims that have gone well? Why did they resolve it quickly. Why was the worker engaged? A comparative analysis of short-versus-long duration claims can be helpful. Look for claims that have similar injury severity but different outcomes.
How Immediate Access to Physician-Led Care Transforms Workers’ Recovery
With modern technology and a focus on treating the whole worker, not just the injury, we can keep injured workers engaged in the recovery process without the risk of getting re-injured after returning to work. The use of telemedicine and 24/7 access to a support program such as JobSiteCare can help companies reduce the risk of extended claim duration and costs. JobSiteCare reduces delays and increases communication. The results are lower claims costs, short claims, and fewer OSHA recordable incidents and DART days.
You can make a difference in the outcome of Workers’ Compensation claims by providing a program that gives your injured workers the opportunity to seek care and treatment as quickly and effortlessly as possible. An effective workplace injury management program should not end with only providing first aid at the job site. It should include modern resources such as telemedicine, which can expand the medical capabilities available to workers without the hassle of traveling off-site and waiting for care at urgent care centers and emergency rooms.
Conclusion
By providing rapid onsite healthcare and case management through telemedicine, you are conveying to your workforce that you care deeply about how a workplace injury is managed. Additionally, you are taking a proactive approach to an area of risk management that is often overlooked. Your broker, carrier, and their underwriters will take notice and see your company as forward-thinking in your risk management strategy.
JobSiteCare aims to support your workers’ compensation efforts by providing timely and effective care, helping reduce both the risk and the cost of workplace injuries. By using our services, you are taking a proactive step to ensure your employees receive the care they need without delay. If you’re looking to enhance your company’s injury management process, please contact us for more information.


